Menstruation Beyond PMS and Ibuprofen

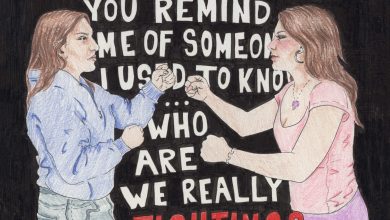
Illustration by Maddy Pease
Periods are generally treated like a monthly visitor to endure with silent acceptance. “Aunt Flo” and other nicknames contribute to the shame swirling around menstruation, relegating conversations to hushed tones and nearly exclusively to cis female spaces. Women are expected to not complain nor address their periods openly, especially to cis men. Menstrual pain is regarded as a fact to accept, or is ignorantly disregarded as a myth conjured by whiny women.
There are many aspects of menstruation that are continuously misunderstood including the basic processes that constitute the menstrual cycle, who experiences menstruation and its symptoms, or which symptoms are “normal” and which are more dangerous.
Few people realize that menstrual pain is considered a medical condition with a given medical term: dysmenorrhea. Even fewer are aware that severe, sometimes debilitating pain can be a sign of more severe medical issues such as endometriosis, a disorder which causes the endometrium (tissue that typically lines the inside of the uterus) to grow outside of the uterus. Endometriosis can lead to fertility issues, cysts, or scar tissue and adhesions. These are legitimate medical conditions that can and should be treated.
Too often, doctors send women home merely telling them to take ibuprofen, invest in a heating pad for their abdomen, and endure each wave of menstrual cramping and pain. Even with the knowledge of more severe disorders, many women with harmful disorders do not get treated long after they bring their symptoms up with a doctor. Women’s pain is commonly overlooked in the medical field; pain stemming from menstruation is further diminished and accepted as a fact of life without much effort invested in helping to treat it.
Beginning with the name itself, birth control has continuously been marketed as a contraceptive to avoid unwanted pregnancies, lending harsh criticism and unnecessary stigma to “the pill.” However, birth control has become an effective medical treatment for many symptoms caused by hormonal fluctuations in the body. Its applications range from treating acne to endometriosis, menstrual cramps to heavy blood flow, and premenstrual syndrome (PMS) to more serious hormonal imbalance syndromes.
Most hormonal birth control primarily regulates the change in levels of estrogen, the primary female sex hormone. Levels of estrogen begin to rise before the period, signaling the body to begin thickening the uterine wall in preparation for an ovum (the female egg ready for fertilization). If the ovum does not get fertilized, then hormone levels drop and the cycle renews once more. These hormonal cycles are important for more than just menstruation, and any irregularities can affect overall health issues such as fatigue and appetite, among others.
The hormonal changes involved in menstruation are further embroiled in misconceptions. Women’s moods are often attributed to PMS, usually in order to invalidate her emotions. However, these accusations (such as “Are you on your rag?”) are wholly inaccurate on top of being sexist. First of all, PMS occurs before menstruation (what is referred to as a period) begins. Secondly, PMS is thought to be caused by the fluctuation in hormones, but can also be exacerbated by brain chemistry and depression. The assumption that women’s periods make them irrationally more moody and upset is false and also unacceptable. PMS can have serious effects on a person’s life, and therefore should not be dismissed as “that thing that makes girls bitchy every month.”
Cis women do not exclusively endure menstruation and the struggles that come with it. Without certain hormone treatments or birth control, transgender men and nonbinary folx can also experience menstruation cycles, including periods. The stigma surrounding periods shames transgender men and nonbinary folx, arguably more than cis women; the masculine rejection of conversation surrounding menstruation can further exacerbate the gender dysphoria experienced by trans men. However, approaching menstruation as a medical condition rather than an inherently feminine experience allows for conversation on how best to handle menstrual cycles.
These conversations have to be had, both in feminine spheres and across demographics. The stigma and misconceptions surrounding periods stem from a denial of the legitimacy of women’s pain. Research must go beyond contraception and focus more on how to best treat the many symptoms of menstruation. Dialogue with doctors must go beyond treating pain as a mild fact of life that over-the-counter drugs can ameliorate. Pain associated with menstruation must be considered a symptom to be investigated fully to rule out any health risks. Menstruation is a medical process and thus can have life-altering consequences for the women and men and nonbinary folx who have to experience it.